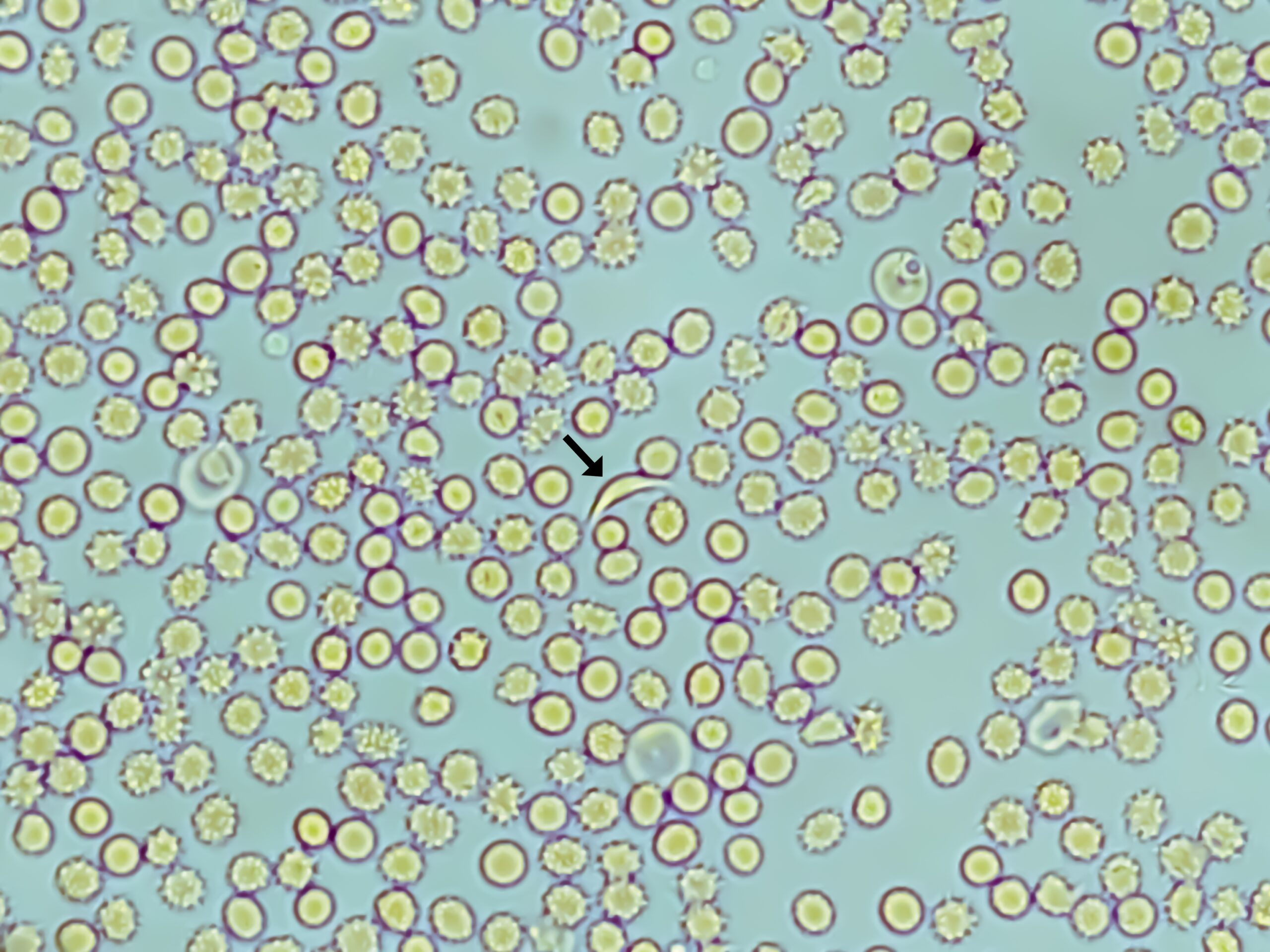
Sickle Cell Disease (SCD) is a genetic blood disorder characterized by the presence of abnormal hemoglobin, leading to the formation of rigid, crescent-shaped red blood cells. While SCD manifests in various ways, one of the most challenging aspects for individuals with this condition is the recurrent and often excruciating pain episodes known as sickle cell pain crises. Understanding the mechanisms underlying pain in Sickle Cell Disease is crucial for developing effective interventions and improving the quality of life for those affected.
The primary mechanism contributing to pain in SCD is vaso-occlusion, a process where sickled red blood cells clump together, obstructing blood vessels and impeding normal blood flow. This blockage can occur anywhere in the body, leading to ischemia, inflammation, and tissue damage. As a result, individuals with SCD experience pain when blood flow is compromised, creating a domino effect of cellular events that contribute to the intensity and duration of sickle cell pain crises.
Ischemia, caused by vaso-occlusion, plays a central role in the genesis of pain in SCD. When tissues and organs do not receive an adequate blood supply, they become deprived of oxygen and essential nutrients. The lack of oxygen triggers the release of inflammatory mediators and signals pain receptors, contributing to the characteristic pain experienced during a sickle cell pain crisis. The severity of the ischemia and the affected organ or tissue determine the intensity and location of the pain.
Inflammation is a key player in the complex mechanisms of pain in Sickle Cell Disease. The interaction between sickled red blood cells, white blood cells, and endothelial cells in blood vessels results in the release of inflammatory cytokines and other mediators. This inflammatory response exacerbates tissue damage and activates pain receptors, intensifying the pain experience. Inflammation also contributes to the chronic nature of pain in SCD, as repeated episodes of vaso-occlusion and tissue damage perpetuate the inflammatory cascade.
Additionally, nerve sensitization plays a role in amplifying pain perception in individuals with SCD. Chronic exposure to inflammatory mediators and repeated pain episodes can lead to changes in the nervous system, heightening the sensitivity of pain receptors. This phenomenon, known as central sensitization, contributes to the persistence and chronicity of pain in SCD. Individuals may experience heightened pain responses to stimuli that would typically be perceived as non-painful.
Psychosocial factors also play a role in the experience of pain in Sickle Cell Disease. The chronic nature of the condition, frequent hospitalizations, and the unpredictability of pain crises can lead to increased stress and anxiety, which, in turn, can exacerbate the perception of pain. Addressing the psychosocial aspects of pain is an integral component of holistic pain management in individuals with SCD.
Understanding the mechanisms of pain in Sickle Cell Disease has paved the way for targeted approaches to pain management. Hydroxyurea, a medication that increases fetal hemoglobin and reduces the frequency of sickle cell pain crises, has demonstrated efficacy in managing pain in individuals with SCD. Other interventions, such as blood transfusions, pain medications, and anti-inflammatory agents, are employed to alleviate symptoms and improve overall quality of life.
Advances in research also highlight the potential of novel therapies, including gene therapies and targeted anti-inflammatory agents, in addressing the underlying mechanisms of pain in Sickle Cell Disease. By targeting specific pathways involved in vaso-occlusion, inflammation, and nerve sensitization, these emerging treatments hold promise for more effective and personalized pain management strategies.
In conclusion, the mechanisms of pain in Sickle Cell Disease are intricate and multifaceted, involving vaso-occlusion, ischemia, inflammation, nerve sensitization, and psychosocial factors. Recognizing the complexity of these mechanisms is essential for tailoring interventions that not only alleviate pain during crises but also address the chronic and recurrent nature of pain in individuals with SCD. Ongoing research and advancements in treatment options offer hope for improved pain management and enhanced quality of life for those navigating the challenges of Sickle Cell Disease.