Neurolytic block techniques represent a specialized area of pain management, primarily used for severe, intractable pain, particularly in cases of cancer pain or chronic pain syndromes. These techniques involve the deliberate destruction or modification of nerve fibers to disrupt pain signal transmission. The rationale behind neurolytic blocks is to provide significant pain relief, improve quality of life, and reduce the need for systemic analgesics, especially opioids, which can have significant side effects.
The most common agents used in neurolytic blocks are alcohol and phenol. Both of these agents cause destruction of nerve fibers, leading to a decrease in pain signal transmission. Alcohol produces its neurolytic effect by extracting cholesterol from neural membranes, leading to the destruction of the nerve. Phenol, on the other hand, causes protein precipitation and coagulation necrosis of neural tissue. The choice between alcohol and phenol often depends on the location of the block and the preference of the practitioner.
One of the most frequently performed neurolytic blocks is the celiac plexus block, used primarily for abdominal pain, particularly in cases of pancreatic cancer. This block targets the celiac plexus, a network of nerves that supply the abdominal organs. By injecting a neurolytic agent into this area, pain signals from the abdomen are significantly reduced. The relief provided by a celiac plexus block can greatly improve a patient’s ability to eat and perform daily activities, thus enhancing their quality of life.
Another common neurolytic procedure is the lumbar sympathetic block, typically used for lower extremity pain, often related to vascular insufficiency or neuropathic conditions like complex regional pain syndrome. This block targets the sympathetic nerves located in the lumbar region, which are part of the autonomic nervous system and play a role in transmitting pain from the lower extremities.
Neurolytic blocks can also be performed at other sites, depending on the source of pain. For example, the stellate ganglion block is used for pain in the head, neck, upper chest, or arm, especially related to nerve injuries, herpes zoster, or cancer. Similarly, intercostal nerve blocks can be used for thoracic pain, such as that caused by rib fractures or thoracotomy.
Despite the benefits, neurolytic blocks are not without risks and complications. The destruction of nerve tissue can sometimes lead to unintended consequences, such as neuritis, deafferentation pain, or motor dysfunction, depending on the location of the block. Therefore, these procedures are generally reserved for situations where the expected benefits outweigh the potential risks. This is especially true in cancer pain management, where the primary goal is often to improve the quality of life for patients with limited life expectancy.
Prior to performing a neurolytic block, a diagnostic block with a local anesthetic is often done. This step helps to predict the efficacy of the neurolytic block and to assess the potential for adverse effects. If the patient experiences significant pain relief with the diagnostic block, it is more likely that a neurolytic block will be effective.
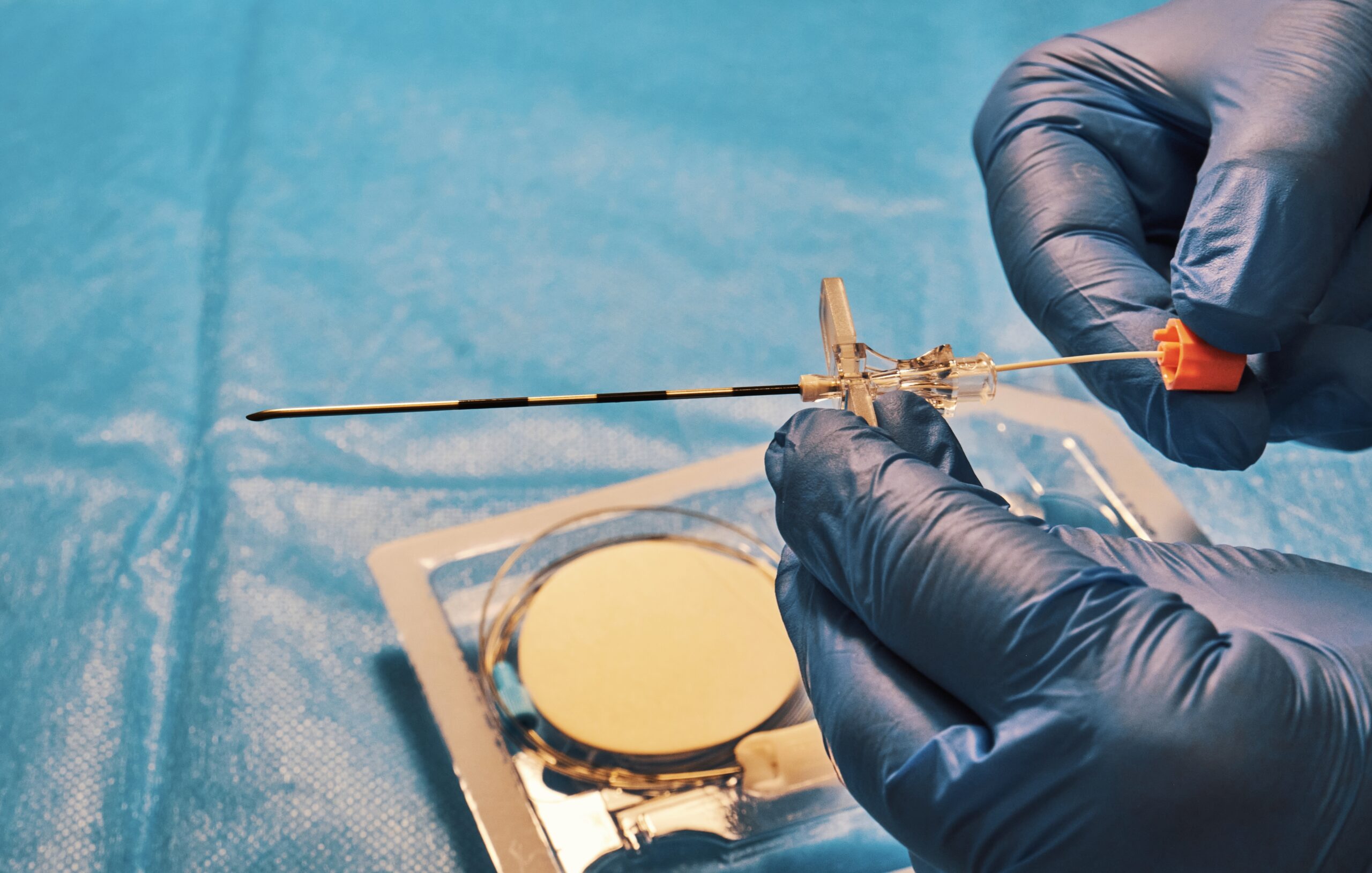
The technique of performing a neurolytic block varies depending on the target nerve or plexus. Typically, the procedure involves the use of imaging guidance, such as fluoroscopy or ultrasound, to ensure accurate placement of the neurolytic agent. This imaging guidance is crucial to avoid damage to adjacent structures and to maximize the efficacy of the block.
In recent years, there has been an increased focus on balancing the benefits of neurolytic blocks with their risks. This has led to the development of more precise techniques and the use of adjunctive therapies to minimize complications. For instance, the use of radiofrequency ablation (RFA) offers a more controlled way to disrupt nerve function, with potentially fewer side effects compared to traditional neurolytic agents.
Neurolytic blocks require a skilled practitioner who is experienced in pain management and the use of interventional techniques. The decision to proceed with a neurolytic block should involve a thorough evaluation of the patient’s pain, general health status, and overall treatment goals. This typically includes a multidisciplinary approach, incorporating input from pain specialists, oncologists, surgeons, and palliative care professionals.
In summary, neurolytic block techniques are a valuable tool in the management of severe, intractable pain, especially in cancer patients. While these procedures can provide significant pain relief and improve the quality of life, they require careful consideration due to their potential risks and complications. Advances in imaging and technique continue to improve the safety and efficacy of neurolytic blocks, making them an important option in the comprehensive management of chronic pain.