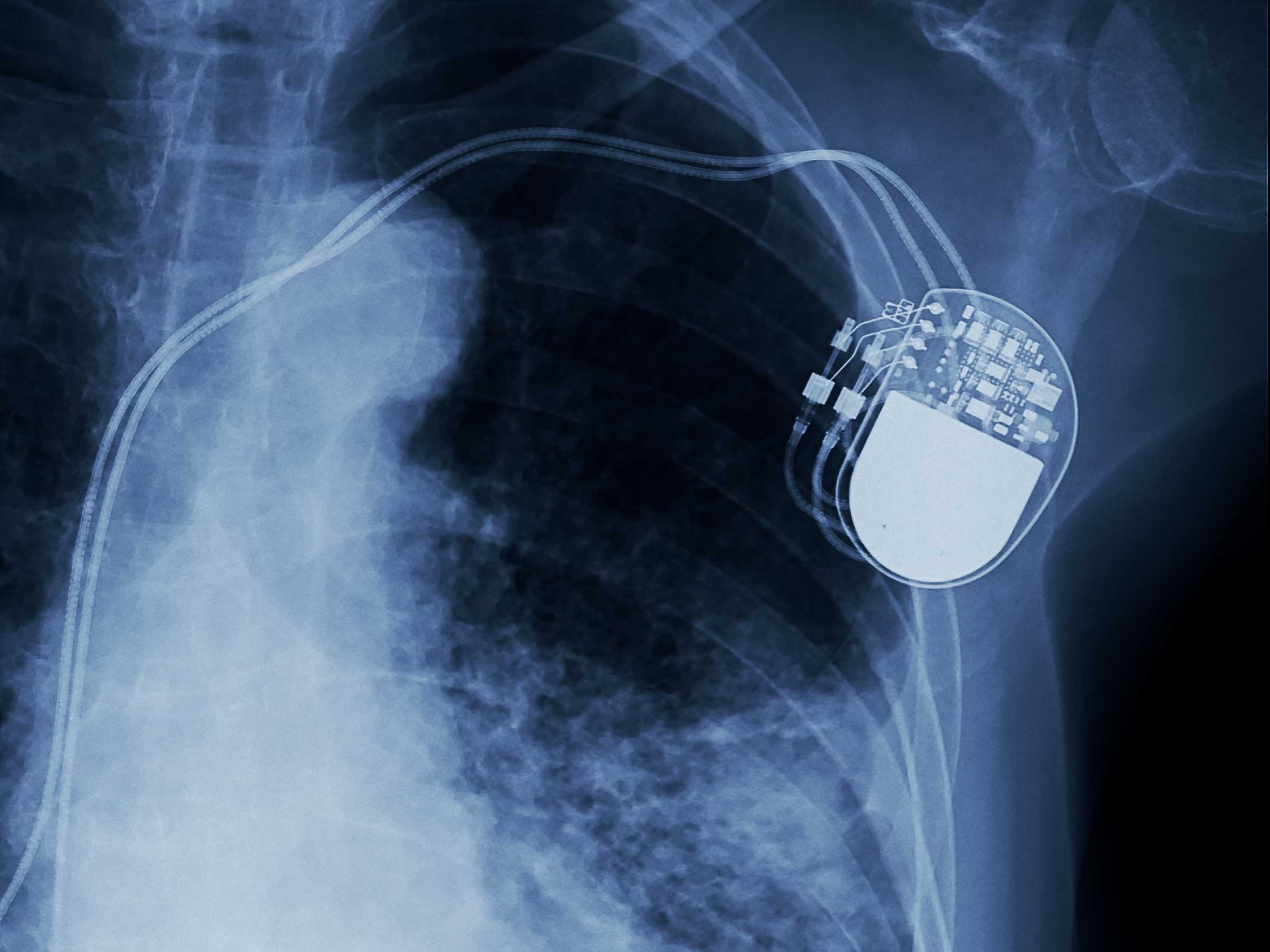
Performing interventional pain management procedures that involve radiofrequency ablation (RFA) in patients with pacemakers or implantable cardioverter-defibrillators (ICDs) requires meticulous planning and care due to potential interactions between the RFA equipment and these cardiac devices. Initially, a thorough pre-procedure assessment is essential, including a detailed medical history focusing on the cardiac condition and an evaluation of the pacemaker or ICD type and settings. Collaboration with a cardiologist or an electrophysiologist is crucial to understand the patient’s cardiac health and device specifics thoroughly. This step is followed by a careful risk-benefit analysis of the RFA procedure.
The planning stage involves forming a multidisciplinary team that includes pain management specialists, anesthesiologists, cardiologists, and technicians experienced in managing cardiac devices. The timing of the procedure is also critical, ideally scheduled when cardiological support is readily available, such as during regular working hours. Managing the cardiac device involves its interrogation and possible temporary reprogramming, such as turning off tachyarrhythmia therapies in ICDs. Continuous monitoring of the device function during the procedure is crucial to detect any malfunctions or setting changes.
During the procedure, comprehensive patient monitoring, including electrocardiography (ECG), blood pressure, and oxygen saturation, is vital. Adjustments in the RFA technique, such as using bipolar radiofrequency probes and careful placement of the grounding pad, are necessary to minimize interference with the cardiac device. Radiofrequency energy should be applied in short bursts at the lowest effective levels to reduce the risk of interference.
Post-procedure care involves immediate re-evaluation of the pacemaker or ICD to ensure it’s functioning properly and returning any settings to their pre-procedure state. Close monitoring of the patient for signs of cardiac complications or device malfunction in the immediate postoperative period is essential. Ensuring the availability of emergency resuscitation equipment and having contingency plans for device failure or cardiac emergencies during the procedure are critical aspects of emergency preparedness.
Informed consent is a key step, where patients are educated about the potential risks and benefits of the procedure, with a focus on considerations specific to their cardiac device. Providing clear post-procedure instructions, including signs of potential complications and when to seek medical help, is part of patient education. It’s also important to document all aspects of the procedure, including device type and settings, procedural details, and any intraoperative events, as well as post-procedure instructions given to the patient and the schedule for follow-up.
Regularly reviewing and updating protocols based on the latest research and clinical guidelines in both pain management and cardiac device management is necessary for continuous improvement. Conducting regular training sessions for staff involved in these procedures ensures they are up-to-date on the latest techniques and safety measures. By adhering to these comprehensive guidelines, healthcare providers can significantly enhance the safety and efficacy of interventional pain management procedures involving radiofrequency ablation in patients with pacemakers and defibrillators, focusing on meticulous planning, interdisciplinary collaboration, and vigilant monitoring to mitigate potential risks and ensure optimal patient outcomes.