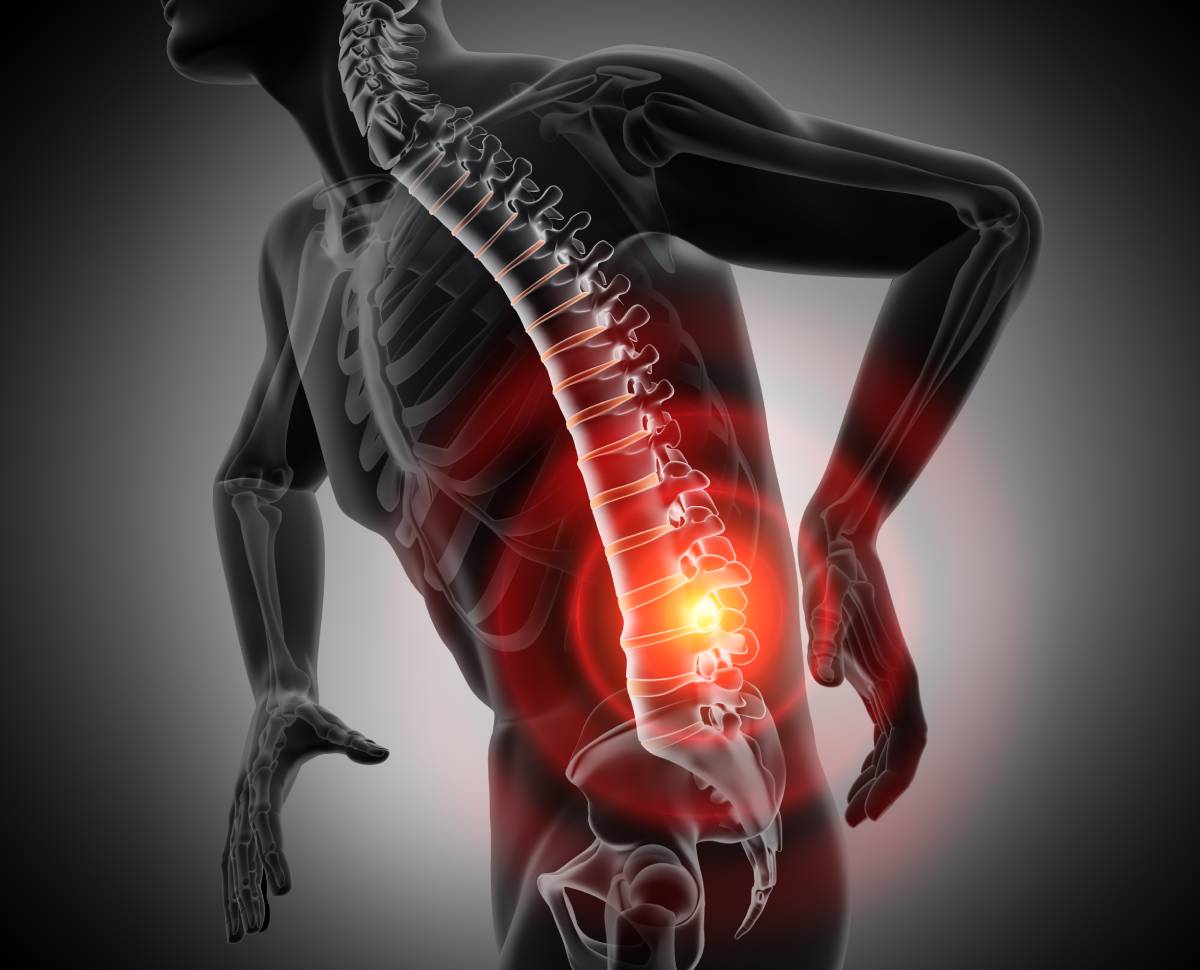
Epidural steroid injections have been a pain management technique since 1952 and are an invaluable non-surgical approach for treating certain spine conditions (1). In particular, they are often recommended for patients with pain that radiates from the lower spine to the hips or legs, or from the neck to arms (1,2). An epidural injection takes advantage of certain aspects of spine anatomy to deliver effective pain relief.
The treatment involves injecting medication into the epidural space to relieve pain caused by inflammation of spinal nerves (1-3). The spinal cord, the ‘highway’ of nerves passing between the body and the brain, is covered by three layers that serve as protection. The outermost and toughest layer is the dura mater. This layer is separated from the vertebrae by the epidural space — literally meaning the space around the dura mater — which contains fat, connective tissue, and spinal nerves (1). Protecting sensitive and delicate nerves is a critical function of many of the components of the spine, as these nerves convey motor signals to the body and sensation from the body. Spinal nerve roots exit the spinal column on each side via the intervertebral foramina, which are the openings between two adjacent vertebrae (1). When nerve passages narrow, the spinal nerve roots can become irritated and inflamed, resulting in pain — patients may also perceive that their pain moves down the arms or legs even though the source of the irritation is at the spine, a phenomenon known as radiating or radicular pain (1,3).
Several conditions can cause pinching and inflammation of the spinal nerves, including herniated discs, bone spurs (including those due to spondylosis), degenerative disc disease, and spinal arthritis (1,3). In herniated discs, the center portion of the disc pushes through the outer layer, placing pressure on the adjacent spinal nerve root. In degenerative disc disease, “the breakdown of intervertebral discs over time may cause the collapse of intervertebral space,” also resulting in compression (1).
Corticosteroids are a type of medication that mimic hormones produced by the body’s adrenal glands to reduce inflammation. They are commonly used to treat arthritis, asthma, autoimmune disorders, and eczema (4). When used in the form of epidural injections, corticosteroids reduce inflammation of affected spinal nerves and open up passages to provide pain relief (1-3). Due to the complex anatomy of the spine, physicians may use X-ray to help guide needle placement into the epidural space during an epidural injection (2,3). Though there are multiple techniques for administering epidural injections, this treatment as a whole has been shown to be safe and to provide pain relief in at least half of patients. The effects usually begin in 1 to 3 days and can last for weeks to months (2).
A successful epidural injection carefully navigates spine anatomy to target the specific location of spinal nerve inflammation to achieve pain relief, thereby “allowing restoration of function” (1). There is also moderate evidence that this treatment reduces the likelihood that patients will require surgery for their pain (5). Patients may also benefit from combining epidural injections with physical therapy, when appropriate, to achieve more sustained pain relief (1).
References
1. Patel, K., Chopra, P., Upadhyayula, S. Epidural Steroid Injections. StatPearls. (Updated July 10, 2020). Available from: https://www.ncbi.nlm.nih.gov/books/NBK470189/
2. “Epidural injections for back pain”. MedlinePlus. (Updated April 21, 2019). Available from: https://medlineplus.gov/ency/article/007485.htm
3. “Epidural Corticosteroid Injections”. Johns Hopkins Medicine. (n.d.). Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/epidural-corticosteroid-injections
4. “Steroids”. MedlinePlus. (Updated June 9, 2020). Available from: https://medlineplus.gov/steroids.html
5. Bicket, M. C., Horowitx, J. M., Benzon, H. T., Cohen, S. P. Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. The Spine Journal. (2014). doi:10.1016/j.spinee.2014.10.011