The use of ultrasound to guide and perform injections for chronic pain management has increased significantly in the past decade and has shown to have many benefits over traditional visualization methods for interventional procedures. While in the past, ultrasound machines were predominantly used for diagnostic imaging, ultrasound has become increasingly popular for use in acquiring venous access1. Some of the other advantages of ultrasound over traditional methods include the ease of performance, absence of ionizing radiation, better visualization of soft tissue (e.g. muscles, ligaments) and blood vessels, real time visualization of needle advancement, and the ability to observe the spread of injectate2. While data suggest that ultrasound guidance may be safer than traditional methods, there are also limits to ultrasound imaging, potentially restricting its role to certain pain management situations3.
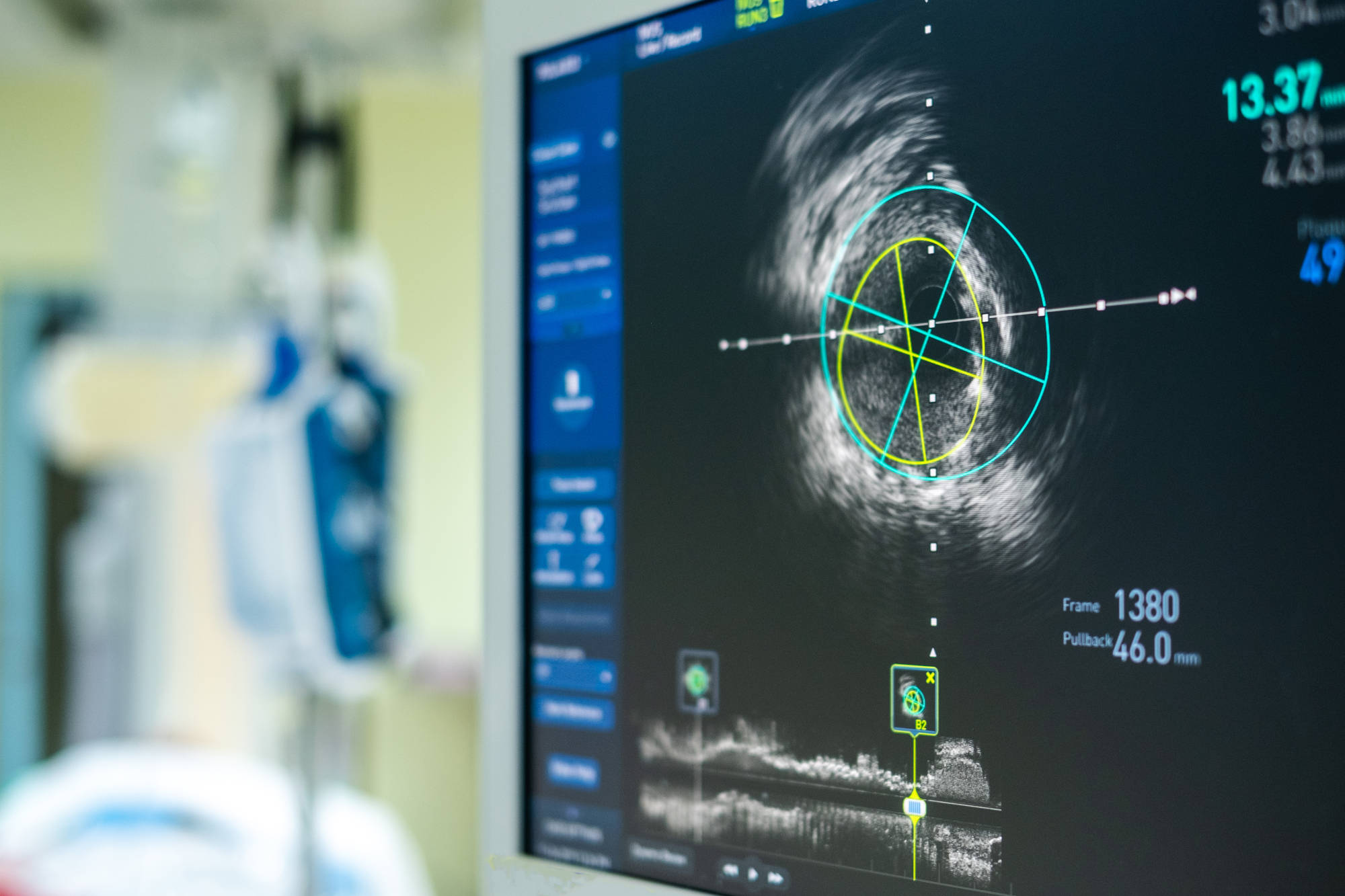
Ultrasound devices work by sending out pulses of vibrations at frequencies beyond the range of human hearing from a probe. These pulses produce echoes from interfaces between tissues of different densities. These echoes can then be used to construct 2D or 3D imaging of the echoing interface4. This mechanism is especially useful for detecting motion: objects moving away from the probe will echo a slightly lower frequency, while objects moving towards the probe will echo a slightly higher frequency. This detection of movement is one of the major advantages of using ultrasound for guided injections, which makes it possible to identify vascular structures.
The types of ultrasound-guided interventional pain injection fall into three groups: neuraxial/spinal, joints, and peripheral/other injections. Depending on the area of injection, ultrasound guided injections are either more effective or equivalent to traditionally guided injections5.
While cost-effective, portable, and more effective for certain injections, there are limits to ultrasound imaging for guided injections. For example, it is particularly difficult to use ultrasound to visualize bone-deep structures, and the overall quality of the images produced is diminished, especially in obese individuals. Additionally, the scarcity of randomized controlled trials demonstrating the effectiveness of ultrasound compared with traditional imaging techniques is a significant barrier to the widespread use of ultrasound. Nonetheless, the advantages of ultrasound use in delineating anatomy and the lack of ionizing radiation (which could otherwise cause tissue damage) bolster the attractiveness of this technique for interventional pain procedures. Together with other imaging modalities, it could improve the safety and accuracy of injections involved in chronic pain management.
Sources:
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst. Rev. 2015 CD006962
- Bhatia A, Brull R. Is ultrasound guidance advantageous for interventional pain management? A systematic review of chronic pain outcomes. Anesth. Analg.2013;117(1):236–251. [PubMed] [Google Scholar]•• A comprehensive review of some of the more popular procedures and evidence that supports their performance under ultrasound (US; or not).
- Narouze SN. Ultrasound-guided interventional procedures in pain management. Reg. Anesth. Pain Med. 2010;35(2 Suppl.):s55–s58. [PubMed] [Google Scholar] [Ref list]
- Terkawi AS, Karakitsos D, Elbarbary M, Blaivas M, Durieux ME. Ultrasound for the anesthesiologists: present and future. Sci. World J.2013;2013:683685. [PMC free article] [PubMed] [Google Scholar]
- Ultrasound-guided interventional procedures for chronic pain management, Samuel Korbe, Esther N Udoji, Timothy J Ness, and Mercy A Udoji, Pain Management 2015 5:6, 466-482