Interventional pain management procedures are an essential component of modern pain management strategies. They aim to alleviate chronic pain and improve patients’ quality of life. Among the various interventions available, corticosteroids play a significant role in managing pain and inflammation. Understanding the appropriate steroid dosing for these procedures is crucial for achieving successful outcomes while minimizing potential risks.
Corticosteroids are potent anti-inflammatory medications that can be administered via various routes, including oral, intravenous, intramuscular, and epidural injections. These drugs mimic the action of natural hormones produced by the adrenal glands and suppress the body’s inflammatory response. In interventional pain management, corticosteroids are commonly used in procedures such as epidural steroid injections, facet joint injections, and sacroiliac joint injections.
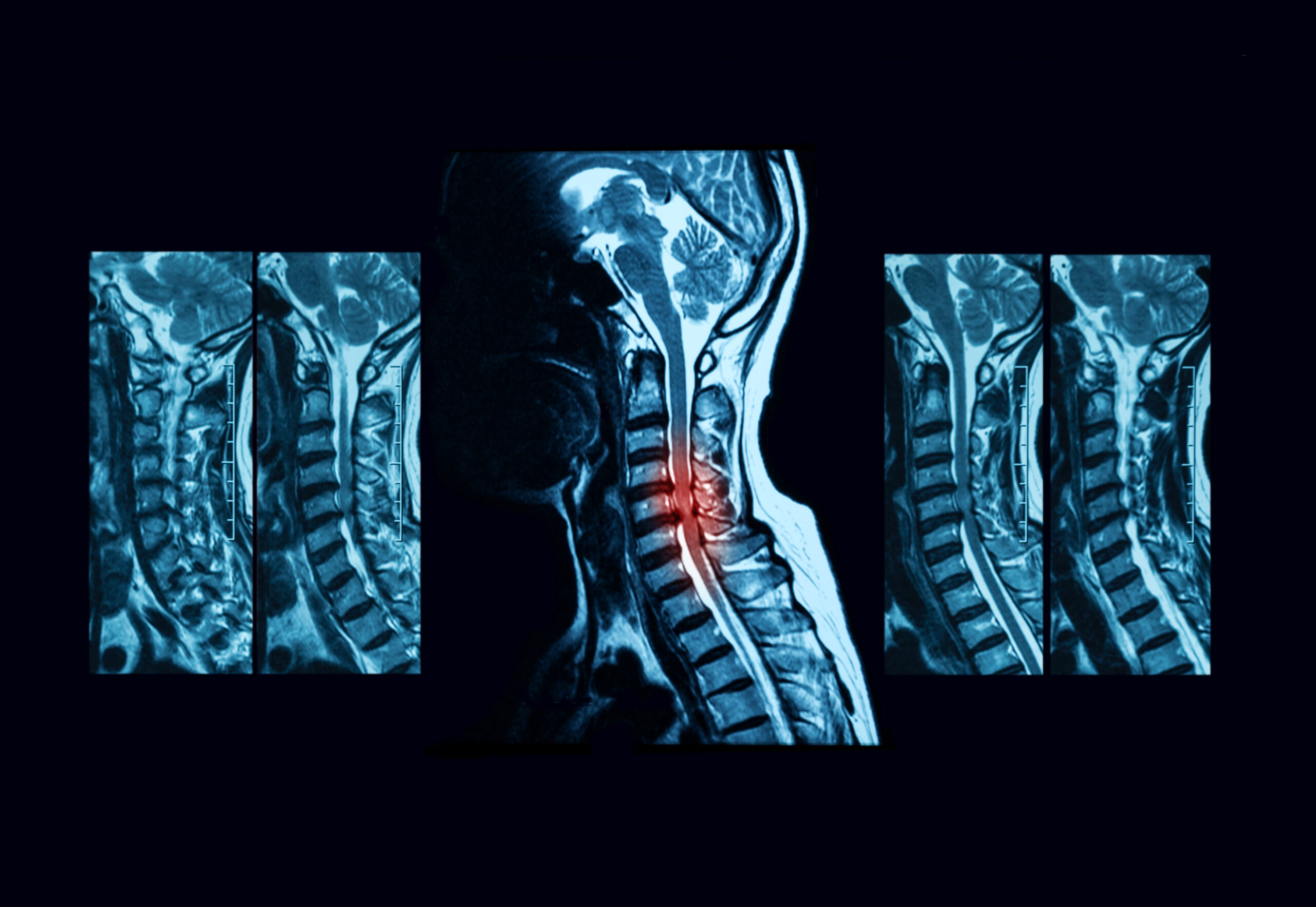
The choice of steroid dosing depends on several factors, including the specific procedure, the patient’s medical history, the severity of the pain, and the duration of symptomatology. A thorough assessment of the patient’s condition, including physical examination and imaging studies, is necessary to determine the most appropriate course of action.
For epidural steroid injections, which are frequently used in the management of radicular pain caused by nerve root compression, corticosteroids are typically combined with local anesthetics. The goal is to reduce inflammation around the affected nerve root and alleviate pain. In this context, an appropriate initial steroid dose may range from 20 to 80 mg of methylprednisolone or an equivalent steroid. However, it is essential to avoid exceeding the recommended cumulative dose to minimize the risk of side effects.
Facet joint injections, employed to manage pain stemming from facet joint arthritis, usually involve the administration of corticosteroids directly into the affected joint. For these procedures, lower doses of steroids, such as 10 to 40 mg of methylprednisolone or an equivalent, are commonly used. Physicians may adjust the dosage based on the patient’s response and consider repeating the procedure if necessary.
Sacroiliac joint injections are performed to alleviate pain originating from the sacroiliac joint, and corticosteroids are often injected directly into the joint space. An appropriate steroid dose for these injections may range from 40 to 80 mg of methylprednisolone or an equivalent steroid.
In all cases, the frequency of interventions is an essential consideration. Repeated injections should be spaced appropriately to prevent the accumulation of steroids and reduce the risk of adverse effects. Typically, a series of injections are administered over weeks or months, depending on the patient’s response and the underlying condition.
It is vital for healthcare providers to be aware of the potential side effects associated with corticosteroid use, particularly with repeated or high-dose administration. Common adverse effects include elevated blood sugar levels, weight gain, mood changes, fluid retention, and increased susceptibility to infections. Additionally, corticosteroids may have adverse effects on bone density, especially with prolonged use.
In conclusion, steroid dosing for interventional pain management procedures requires a careful balance between achieving pain relief and minimizing potential risks. Healthcare providers must tailor the steroid dose to each patient’s unique needs, taking into account their medical history, the specific procedure being performed, and the desired outcomes. Regular follow-up and close monitoring of patients are essential to ensure that the benefits of steroid treatment outweigh any potential drawbacks, ultimately optimizing the success of interventional pain management interventions.