Lumbar epidural steroid injections (LESIs) are a means of assuaging lumbar radiculopathy, which involves numbness, muscle weakness, tingling, or even pain radiating down from the lower back to the hips, legs, and possibly feet [1]. Because lumbar radiculopathy can be caused by many conditions —among them lumbar degenerative disk disease, lumbar spinal stenosis, and lumbar osteoarthritis—, LESIs may not be equally effective for treating pain across patient presentations [1]. Furthermore, the safety of this type of injection has previously been up for debate among the medical community [2]. Consequently, medical practitioners should consider the efficacy and safety of lumbar epidural steroid injections before performing this procedure on patients.
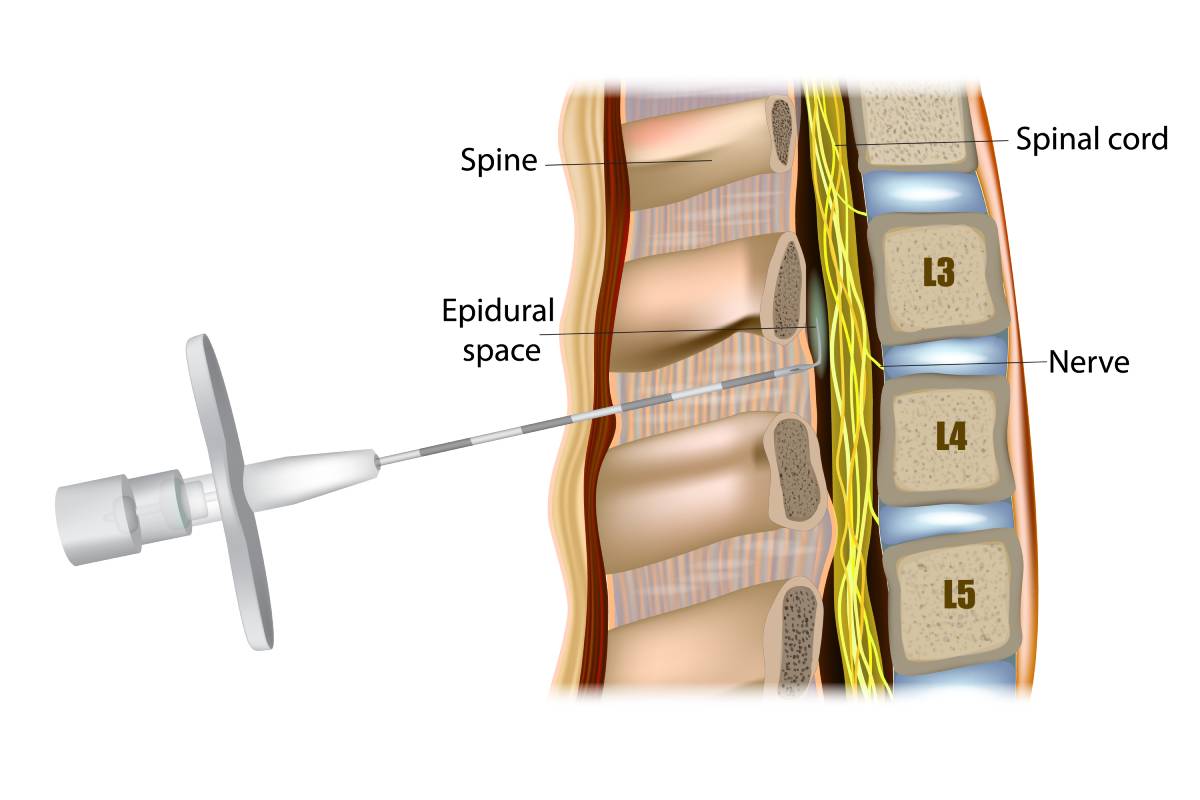
Generally, to perform a LESI, the provider will inject the patient with an anti-inflammatory substance, typically a corticosteroid or a steroid, in the epidural space around the spinal nerves [1]. Practitioners can choose between various ways of accessing the epidural space: some opt for caudal epidural spinal injection (ESI), guiding the needle through the sacral hiatus to reach the lowest spinal nerves, while others may choose the interlaminar ESI, pushing the needle between the two spinal lamiae, or the transforaminal ESI, which involves the needle going through the foramina [1]. Regardless of the entrance route, the procedure, on the whole, tends to be brief, taking only about 15 to 30 minutes [1].
Researchers have identified differences in efficacy between injection routes. For instance, Pandey compared the caudal, interlaminar, and transforaminal methods across 152 patients and found that, while all three were generally effective in treating patients’ low back pain, they observed the best results among the 40 patients who received a transforaminal injection [3]. More precisely, the transforaminal route more effectively treated patients’ pain levels in the half-year and year following the injection [3]. Similarly, Manchikanti et al. conducted a meta-analysis of three randomized controlled trials and found that all three routes were effective, with higher rates of improvement observed in the transforaminal group [4].
Concerning safety, post-LESI complications tend to be rare [1]. Although the U.S. Food and Drug Administration once warned that corticosteroid injections in the epidural space could lead to serious events in rare instances, such as stroke, paralysis, or death, spinal epidural injections tend to be safe in practice [2, 5]. A seven-year retrospective analysis analyzing 1,857 patients identified a 2.4% incidence rate of complication per injection [5]. The complications reported tended to be minor: they were persistent numbness, pain at the injection site, increased pain, or “other” [5]. Most of the 4,265 injections documented within the group were lumbar transforaminal injections (3,964) [5]. These findings were consistent with other studies reporting a paucity of serious complications among ESI patients [2, 6]. Certainly, researchers have documented long-term complications such as bleeding, infection, neurologic issues, and endocrine effects among epidural spinal injection patients but, again, they are rare [5].
Chronic low back pain contributes to high rates of disability worldwide and, consequently, a substantial individual, economic, and social burden [Pandey]. Because of their demonstrated efficacy and safety in treating chronic low back pain, lumbar spinal epidural injections are useful for combating this widespread phenomenon and helping improved patients’ quality of life.
References
[1] “Lumbar Epidural Steroid Injection,” Cleveland Clinic, Updated November 19, 2021, [Online]. Available: https://my.clevelandclinic.org/health/treatments/22091-lumbar-epidural-steroid-injection.
[2] D. J. Kennedy et al., “Epidural Steroid Injections are Safe and Effective: Multisociety Letter in Support of the Safety and Effectiveness of Epidural Steroid Injections,” Pain Medicine, vol. 16, no. 5, pp. 833-838, May 2015. [Online]. Available: https://doi.org/10.1111/pme.12667.
[3] R. A. Pandey, “Efficacy of Epidural Steroid Injection in Management of Lumbar Prolapsed Intervertebral Disc: A Comparison of Caudal, Transforaminal and Interlaminar Routes,” Journal of Clinical & Diagnostic Research, vol. 10, no. 7, pp. RC05-RC11, July 2016. [Online]. Available: https://doi.org/10.7860%2FJCDR%2F2016%2F18208.8127.
[4] L. Manchikanti et al., “Comparison of the Efficacy of Caudal, Interlaminar, and Transforaminal Epidural Injections in Managing Lumbar Disc Herniation: Is One Method Superior to the Other?,” The Korean Journal of Pain, vol. 28, no. 1, pp. 11-21, January 2015. [Online]. Available: https://doi.org/10.3344%2Fkjp.2015.28.1.11.
[5] J. H. Jung et al., “Long-Term Complications of Epidural Steroid Injections,” Current Physical Medicine and Rehabilitation Reports, vol. 2, pp. 55-60, January 2014. [Online]. Available: https://doi.org/10.1007/s40141-013-0038-6#auth-Lysander-Jim.
[6] M. Benoist, P. Boulu, and G. Hayem, “Epidural steroid injections in the management of low-back pain with radiculopathy: an update of their efficacy and safety,” European Spine Journal, vol. 21, pp. 204-213, September 2011. [Online]. Available: https://doi.org/10.7860%2FJCDR%2F2016%2F18208.8127.