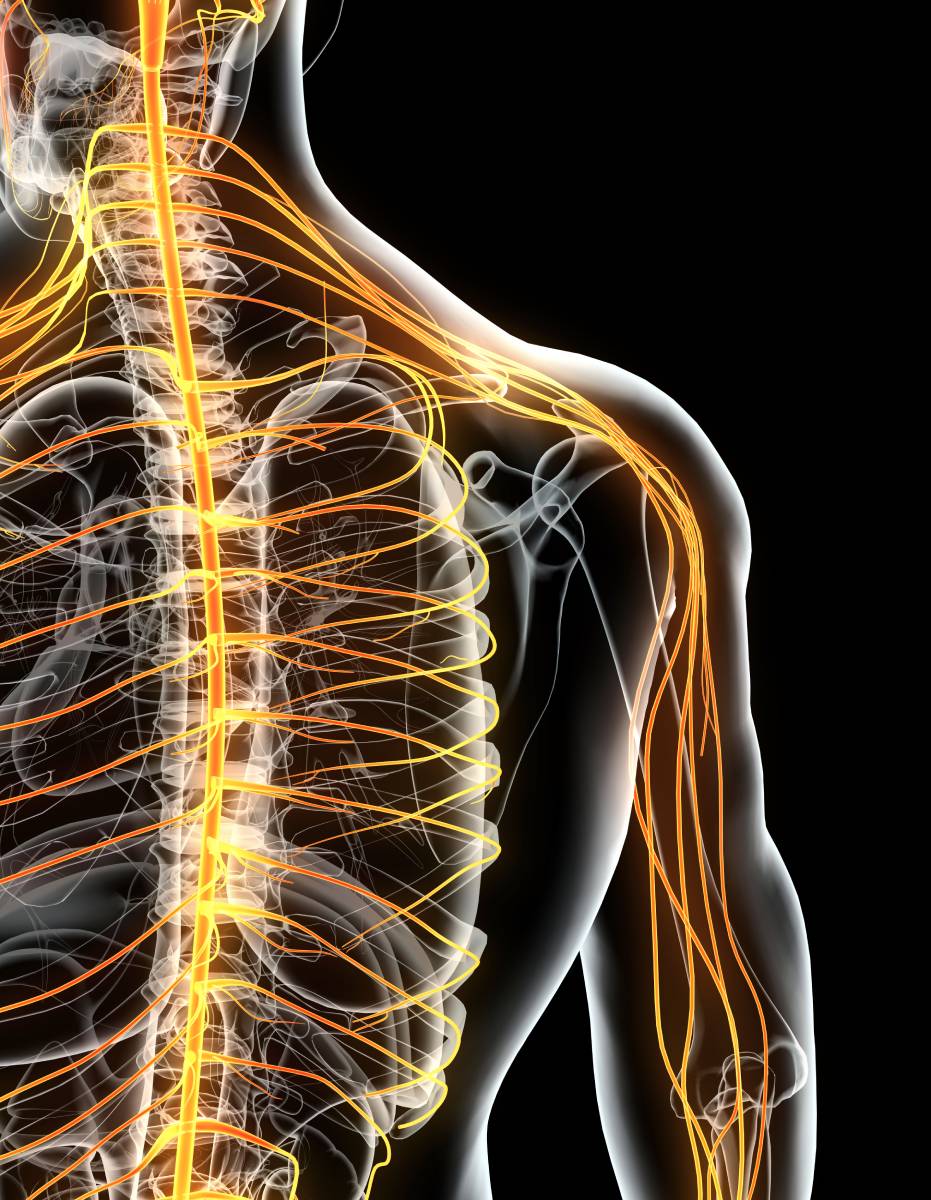
The nervous system recognizes, transmits, and processes the sensation of pain. Sensory nerves throughout the body are responsible for detecting pain, as well as touch, temperature, and position, and then these signals are carried back to the spinal cord and brain (comprising the central nervous system). Meanwhile, motor commands are carried by motor nerves from the central nervous system to the muscles involved. The spinal column is a key structure in these processes, and our understanding of the anatomy and organization of spinal nerves has advanced the diagnosis and treatment of painful conditions related to spinal nerves, as well as the field of anesthesia and pain control.
Spinal nerves exist in pairs, emerging from the left and right sides of the spine. They connect the central nervous system to peripheral tissues and have sensory, motor, and autonomic functions. At each level, one dorsal (posterior), sensory root and one ventral (anterior), motor root join together on either side of the spine to form a spinal nerve, which innervates a particular region of the body (1,2). Note, however, that the sensory innervation area – the dermatome – and the motor innervation area – the myotome – of a particular spinal nerve do not necessarily overlap completely (2).
There are 31 pairs of spinal nerves, with 8 in the cervical region of the spine, 12 in the thoracic region, 5 in the lumbar region, and 1 in the coccygeal region. Generally speaking, the dermatome and myotome of a pair of spinal nerves aligns logically with the body’s anatomy – those in the cervical region innervate the nearby areas of the scalp, neck, and chest; those in the thoracic region innervate the nearby areas of the back, abdomen, and gut; and those in the lumbar region innervate the pelvis and lower body. Some spinal nerves merge with each other to form a “plexus” (1,2).
The organized nature of spinal nerve anatomy has significant implications for medicine. For example, in the context of anesthesia, peripheral nerve blocks target specific spinal nerves or groups of spinal nerves to block pain sensation from a specific region of the body. This technique is increasingly used to control postoperative pain, as well as chronic pain in a few situations. Surgery on an upper extremity may involve a brachial plexus block, while lower extremity surgery may involve a femoral block, for example (3).
Spinal nerve anatomy also is key to understanding, diagnosing, and treating many conditions of the spine that can cause chronic pain. Radiculopathy is a common condition that is characterized by a pinched spinal nerve, and symptoms vary by the location of the underlying issue. Cervical radiculopathy typically causes pain, weakness, and/or numbness in the arms and hands, areas that are innervated by cervical spinal nerves. Similarly, thoracic radiculopathy (the least common form) can cause symptoms in the trunk; lumbar radiculopathy can cause symptoms in the legs (4). Interestingly, different types of disc herniations at the same level may affect different spinal nerves. This is because, lower in the spine, nerve roots tend to travel downward before exiting between vertebrae – as a result, lateral disc herniations are more likely to affect nerves that are exiting at that level, whereas paracentral disc herniations are more likely to affect nerves that exit at a lower level (1).
The mapping of spinal nerves in the context of the overall body’s anatomy greatly impacts pain and analgesia. However, research has also identified anatomical variations in a minority of the population, with implications for the medical care of such patients (1,2).
References
- Kaiser JT, Lugo-Pico JG. Neuroanatomy, spinal nerves. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Updated 2021. Available: https://www.ncbi.nlm.nih.gov/books/NBK542218/
- Moawad H. “The Anatomy of Spinal Nerves,” VerywellHealth. Updated April 1, 2021. Available: https://www.verywellhealth.com/spinal-nerves-anatomy-4682599
- Joshi G, Gandhi K, Shah N, Gadsden J, Corman SL. Peripheral nerve blocks in the management of postoperative pain: challenges and opportunities. Journal of Clinical Anesthesia. 2016, 35, 524-529. DOI:10.1016/j.jclinane.2016.08.041
- “Radiculopathy,” Johns Hopkins Medicine. N.d. Available: https://www.hopkinsmedicine.org/health/conditions-and-diseases/radiculopathy