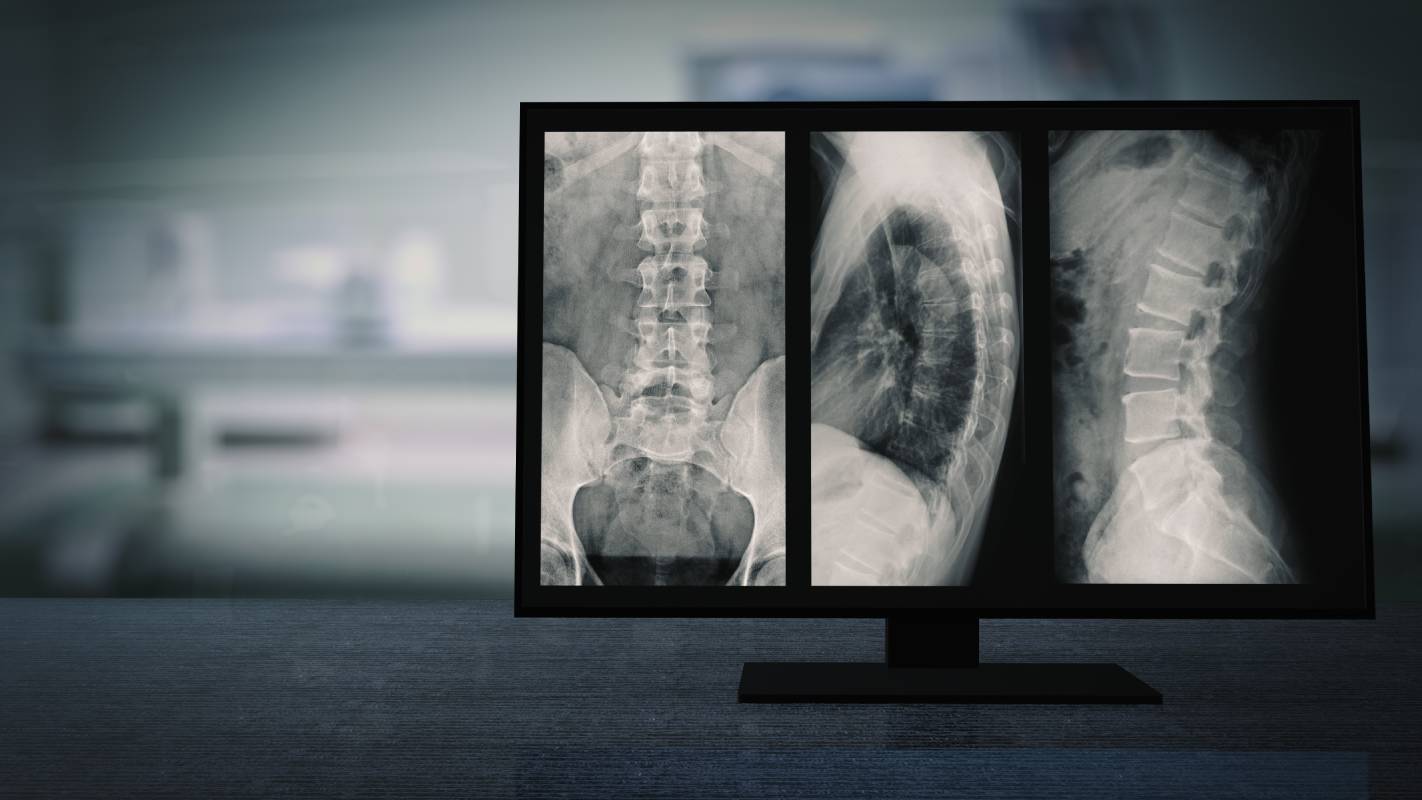
As people age, the spine undergoes several changes [1]. These changes include decreases in mineral density, degeneration of various facets of the spine, and misalignment [1, 2]. These processes do not occur at equal paces, and their respective severity can differ across people, but many of them often contribute to pain and/or debilitation [1, 3]. This article will explore the various changes to the spine that occur with age, and the conditions that arise as a result of those transformations.
One of the most common age-related spine changes is degeneration [1]. One type of degeneration is intervertebral disk degeneration, which can result in increased concentrations of proteolytic enzymes, disrupted collagen fiber organization, and water and glycoprotein loss [1] As a result, vessels and nerves may penetrate the normally avascular nucleus of the disk and, accordingly, trigger a mutually reinforcing cycle of inflammation and further degeneration [1]. Another common product of disk degeneration is severe pain [1]. Although disk degeneration is just one form of weathering that occurs with age, facet and ligament joint degeneration are also possible [1]. Together, these three forms of degeneration impair the body’s ability to forward translate the vertebra, which can spur the development of degenerative spondylolisthesis [1].
Another common result of aging on the spine is alterations in disk height [4]. Disk height is closely related to spinal degeneration, given that degeneration generally results in decreased disk height, as well as a decrease in disk volume and less concave disk shape [4]. To investigate the extent of disk height change among older people, Pfirrmann and colleagues studied 70 asymptomatic volunteers ranging from 20 to 78 years old [4]. The researchers identified the expected negative correlations between shape characteristics and degenerations, but interestingly, a positive correlation between age and disk height in the absence of degeneration [4].
As for cervical alignment, researchers have pinpointed some associations between changes to particular spine regions and age. For instance, Iorio et al. conducted three-dimensional biplanar imaging of 118 subjects [2]. They found that C0-CY and C2-C7 lordosis tended to increase with age, but, contrary to their hypothesis, there was no association between C0-C2 angle and age [2]. Meanwhile, Liu and colleagues found that cervical angle, neck tilt, and thoracic inlet angle all tended to rise with age [5]. Noting how cervical spine misalignment increases pressure on adjacent portions of the intervertebral disc, these changes can reinforce degeneration and result in severe conditions like cervical degenerative disease [5].
Relatedly, Langella et al. conducted a retrospective cohort study to clarify the relationship between kyphotic fractures, spinal alignment, and quality of life in elderly populations [6]. Research indicates that spinal malalignment is strongly associated with kyphotic fractures and spinal deformity [6]. Unfortunately, both conditions become more prevalent with age and, consequently, are frequent causes of spinal morbidity in the elderly [6]. In this experiment, the researchers concluded that sufferers of kyphotic vertebral fractures are more likely to suffer from sagittal spinal alignment and perceived disability as well [6].
With age, people are more susceptible to high degrees of pain, disease, and disability because of their changing spines. Although surgery and medications can alleviate the negative effects of these conditions, age-related spine changes can still take a significant toll on elderly people.
References
[1] M. Papadakis et al., “Pathophysiology and Biomechanics of the Aging Spine,” The Open Orthopaedics Journal, vol. 5, p. 335-342, September 2019. [Online]. Available: https://doi.org/10.2174/1874325001105010335.
[2] J. Iorio et al., “The Effect of Aging on Cervical Parameters in a Normative North American Population,” Journal of Orthopaedic Research, vol. 8, no. 7, p. 709-715, March 2018. [Online]. Available: https://doi.org/10.1177/2192568218765400.
[3] F. Johannesdottir et al., “Population-based study of age- and sex-related differences in muscle density and size in thoracic and lumbar spine: the Framingham study,” Osteoporosis International, vol. 29, p. 1569-1580, March 2018. [Online]. Available: https://doi.org/10.1007/s00198-018-4490-0.
[4] C. W. A. Pfirrmann et al., “Effect of aging and degeneration on disc volume and shape: A quantitative study in asymptomatic volunteers,” Journal of Orthopaedic Research, vol. 24, no. 5, p. 1086-1094, April 2006. [Online]. Available: https://doi.org/10.1002/jor.20113.
[5] J. Liu et al., “The effects of aging on the profile of the cervical spine,” Medicine, vol. 98, no. 7, p. 1-5, February 2019. [Online]. Available: https://doi.org/10.1097/MD.0000000000014425.
[6] F. Langella et al., “The aging spine: the effect of vertebral fragility fracture on sagittal alignment,” Archives of Osteoporosis, vol. 16, no. 109, p. 21-32, July 2021. [Online]. Available: https://doi.org/10.1077/s11657-021-00975-w.