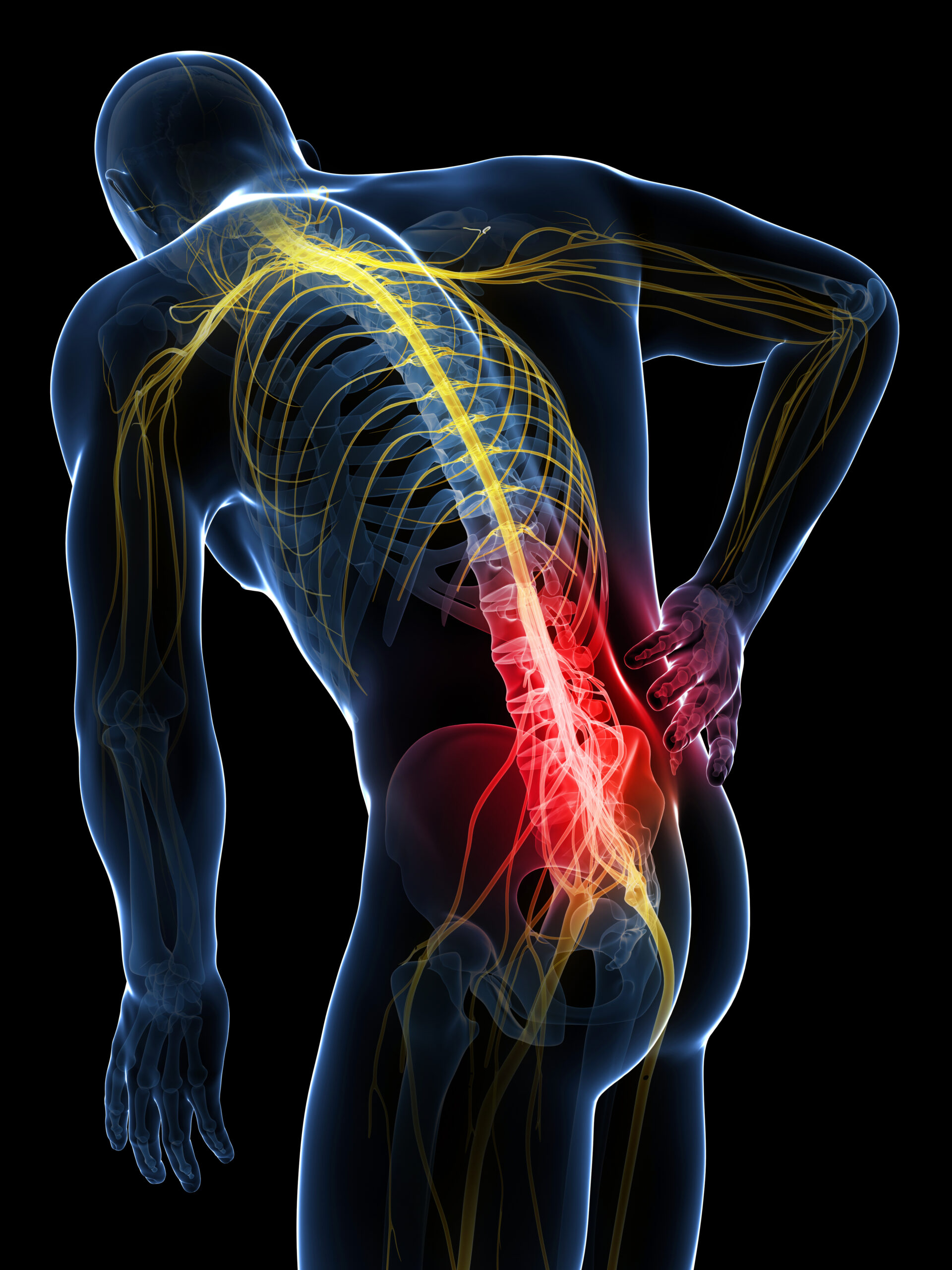
Peripheral nerve stimulation (PNS) has emerged as a promising therapeutic approach for managing chronic pain. One area of particular interest is the stimulation of the cluneal nerve, which is often implicated in lower back pain and other related conditions. The cluneal nerve, specifically the superior cluneal nerve, can be a source of significant discomfort due to its anatomical course and susceptibility to entrapment. This essay explores the anatomy of the cluneal nerve, the principles and mechanisms of peripheral nerve stimulation, the clinical applications of PNS for cluneal nerve pain, and the outcomes and potential future directions of this treatment modality.
Anatomy of the Cluneal Nerve
The cluneal nerves are a group of nerves that provide sensory innervation to the skin of the buttocks. They are divided into three groups: the superior, middle, and inferior cluneal nerves. The superior cluneal nerves, which are most commonly associated with chronic pain, arise from the dorsal rami of the L1 to L3 spinal nerves. These nerves travel through the lumbar region and pass over the iliac crest, where they can become entrapped or irritated.
The superior cluneal nerves innervate the upper part of the buttocks and are particularly prone to entrapment as they pass through the thoracolumbar fascia and over the iliac crest. This entrapment can lead to a condition known as superior cluneal nerve entrapment syndrome, characterized by localized pain in the lower back and buttocks. This condition is often underdiagnosed, leading to chronic pain that can significantly impact a patient’s quality of life.
Principles and Mechanisms of Peripheral Nerve Stimulation
Peripheral nerve stimulation involves the application of electrical impulses to a targeted nerve to modulate its activity. This technique can provide pain relief by interrupting the transmission of pain signals to the brain and by stimulating the release of endogenous pain-relieving substances. PNS is typically achieved through the implantation of a small electrode near the nerve, connected to a pulse generator that delivers controlled electrical impulses.
The mechanisms by which PNS alleviates pain are multifaceted. One primary mechanism is the gate control theory of pain, which suggests that non-painful stimuli can inhibit the transmission of painful signals in the spinal cord. Electrical stimulation of the cluneal nerve can activate large-diameter sensory fibers, which in turn inhibit the transmission of pain signals carried by smaller, pain-conducting fibers.
Additionally, PNS may enhance the release of endogenous opioids and other neurotransmitters that modulate pain perception. The stimulation can also reduce hyperexcitability of neurons in the dorsal horn of the spinal cord, further diminishing pain sensation.
Clinical Applications of PNS for Cluneal Nerve Pain
Peripheral nerve stimulation has been increasingly used for managing chronic pain conditions, including those involving the cluneal nerve. Patients with superior cluneal nerve entrapment syndrome often present with chronic lower back pain that is resistant to conventional treatments such as medications, physical therapy, and nerve blocks. For these patients, PNS offers a potential alternative or adjunctive treatment.
The process begins with a thorough diagnostic evaluation to confirm the involvement of the cluneal nerve. This often includes a detailed clinical history, physical examination, and diagnostic nerve blocks. Once the diagnosis is confirmed, a trial of PNS may be initiated. During the trial, a temporary electrode is implanted near the cluneal nerve, and the patient’s response to stimulation is monitored. If significant pain relief is achieved, a permanent system can be implanted.
The implantation procedure for PNS is minimally invasive and typically performed under local anesthesia. An electrode is placed near the cluneal nerve, and a pulse generator is implanted in a subcutaneous pocket, usually in the lower back or buttock region. The pulse generator can be programmed to deliver electrical impulses according to the patient’s needs, providing customizable pain relief.
Outcomes and Benefits of PNS for Cluneal Nerve Pain
Clinical studies and case reports have demonstrated the efficacy of PNS for managing cluneal nerve pain. Patients often experience significant reductions in pain intensity, improved function, and enhanced quality of life. One of the key benefits of PNS is its ability to provide targeted pain relief with minimal side effects compared to systemic medications.
For patients with cluneal nerve entrapment syndrome, PNS can offer sustained pain relief, allowing them to engage in daily activities and physical therapy more effectively. This improvement in functional capacity can lead to better overall outcomes and reduced reliance on pain medications, which can have adverse effects when used long-term.
Moreover, PNS is a reversible and adjustable treatment. If the patient’s pain pattern changes or if there are issues with the device, the settings can be adjusted non-invasively, and the system can be removed if necessary without permanent alterations to the body.
Future Directions and Considerations
The use of PNS for cluneal nerve pain is still evolving, with ongoing research aimed at optimizing techniques, improving device technology, and understanding the long-term outcomes. Advances in neurostimulation technology, such as wireless systems and closed-loop feedback mechanisms, hold promise for enhancing the effectiveness and convenience of PNS.
Furthermore, the identification of specific patient characteristics that predict positive responses to PNS can help tailor treatment to those most likely to benefit. This personalized approach can maximize the therapeutic benefits of PNS and minimize unnecessary procedures.
Despite its benefits, PNS is not without challenges. The cost of the devices and the implantation procedure can be significant, and there may be limitations in insurance coverage. Additionally, like any medical procedure, there are risks associated with implantation, such as infection, device migration, and hardware malfunction.
Conclusion
Peripheral nerve stimulation represents a valuable tool in the management of chronic pain associated with the cluneal nerve. Its ability to provide targeted, adjustable, and reversible pain relief makes it a promising option for patients with superior cluneal nerve entrapment syndrome and other related conditions. As technology advances and our understanding of peripheral nerve stimulation deepens, its role in pain management is likely to expand, offering hope to many individuals suffering from chronic pain conditions.